Rush Prudential HMO, Inc. v. Moran
United States Supreme Court
536 U.S. 355, 122 S. Ct. 2151, 153 L. Ed. 2D 375 (2002)
- Written by Craig Conway, LLM
Facts
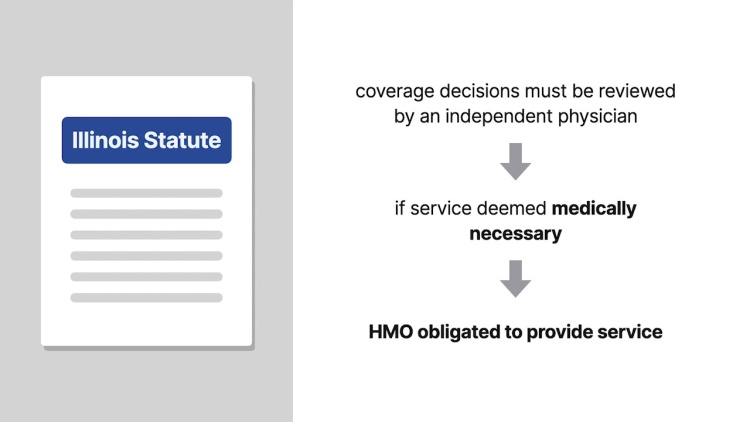
Rush Prudential HMO, Inc. (Rush) (defendant) contracted with employers to provide medical services for employee welfare benefit plans covered by the federal Employment Retirement Income Security Act of 1974 (ERISA). Rush promised to pay for “medically necessary” services performed by a list of primary care physicians and other health care providers. Rush would pay for medically necessary services performed by physicians not on Rush’s list if the primary care physician and Rush’s medical director approve the services. Debra Moran (plaintiff) was covered under Rush’s plan. In 1996, Moran began experiencing pain in her shoulder. Her primary care physician, Dr. Arthur LaMarre, recommended that Rush approve a surgical procedure to be performed by a specialist unaffiliated with Rush. Rush denied Moran’s request for the procedure on the basis that it was not “medically necessary.” In January 1998, Moran demanded that Rush provide an independent medical review of her claim as guaranteed under § 4-10 of Illinois’ HMO Act. When Rush failed to provide the independent review, Moran sued Rush in Illinois state court to compel compliance with the state law. Rush requested removal to federal district court arguing that her cause of action was completely preempted under ERISA. While the suit was pending, Moran had the surgery, and submitted a $94,841.27 reimbursement to Rush. Treating the request as a new claim, Rush consulted three physicians who unanimously agreed that Moran’s surgery was medically unnecessary. The federal court remanded the matter back to state court on Moran’s motion, holding that her request for an independent review was not preempted by ERISA. The state court found in favor of Moran and ordered Rush to furnish the independent review. An independent physician concluded that the surgery was medically necessary. However, Rush’s medical director still held the surgery medically unnecessary and denied Moran’s reimbursement request. Moran amended her complaint in state court to seek reimbursement for the surgery under Illinois’s HMO Act. Rush requested removal to federal court arguing again that the claim concerned ERISA benefits and thus was completely preempted. The district court agreed that the claim was preempted and ruled that Illinois’s independent review statute was preempted and thus unenforceable. Moran appealed and the court of appeals reversed. The United States Supreme Court granted certiorari.
Rule of Law
Issue
Holding and Reasoning (Souter, J.)
Dissent (Thomas, J.)
What to do next…
Here's why 907,000 law students have relied on our case briefs:
- Written by law professors and practitioners, not other law students. 47,100 briefs, keyed to 996 casebooks. Top-notch customer support.
- The right amount of information, includes the facts, issues, rule of law, holding and reasoning, and any concurrences and dissents.
- Access in your classes, works on your mobile and tablet. Massive library of related video lessons and high quality multiple-choice questions.
- Easy to use, uniform format for every case brief. Written in plain English, not in legalese. Our briefs summarize and simplify; they don’t just repeat the court’s language.